Pulmonary tuberculosis is by far the most common manifestation of TB witnessed throughout the Stannington records. Prior to the development and use of any effective antibiotic treatments the most common form of intervention was the induction of an artificial pneumothorax. Many of the different treatments employed to treat TB of all types at this time were based on the principles of resting and isolating the affected area, and the thinking behind artificial pneumothorax treatment was no different.
A needle would be inserted through the chest wall to allow for the insertion of air into the pleural cavity. The amount of air inserted would depend on the size of the patient as well as how much the physician in charge though the patient could realistically manage in one go and how quickly they wished the lung to collapse. Once inserted the pressure from the air would force the lung to collapse in on itself and to cease functioning properly. The entire lung would not necessarily be collapsed at once, either because it wasn’t necessary for treatment or because fibrotic adhesions between the lung and the chest wall as a result of the disease prevented it from doing so. Where only part of the lung was affected it would not be desirable to collapse the whole lung and in such instances just one lobe might be collapse. Bilateral artificial pneumothorax was also a possibility, whereby part of both lungs would be collapsed at the same time. A state of collapse could be maintained for a period of months or even years and required the patient to undergo regular refills of air in order to do so.
A great number of radiographic illustrations of the progression of a collapse are available in the Stannington collection. One patient, 2/1946, has a large amount of radiographs taken over a period of two years which demonstrate the change in the lung from admission and through the progressive stages of lung collapse.
Patient 2/1946 was female an age15 when she was admitted to Stannington on 21 June 1945 with pulmonary TB stage 3, at which point her sputum tested positive for TB also. A report on an x-ray taken pre-admission reads:
‘Right lung shows several active foci beginning to coalesce. There is extensive infiltration in the upper zone & suspicious blotchy areas in the middle zone. A small calcified opacity in the right lower zone. The left lung shows infiltration in the middle zone. The upper zone and apex are clear. Early active foci are noticeable in both lungs in the affected areas.’
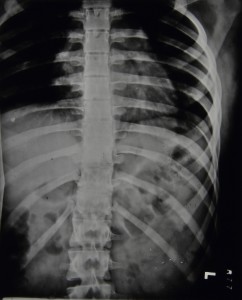
Figure 1 was the first x-ray taken after admission on 25 June 1945 being three weeks later than the one reported above. Observations on this x-ray note:
‘Scattered foci in right upper zone. One definite cavity. Increased bronchial marking at both bases.’

25 June 1945

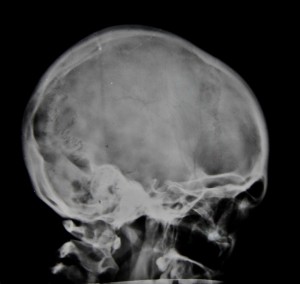
31 Aug 1945
It was quickly decided that and artificial pneumothorax should be induced on the right side and this took place on 16 Aug 1945. Figure 2 taken later on that month shows the initial results of the artificial pneumothorax. The black area along the lateral side of the right lung is evidence of the air that has been inserted and the lung has begun to compress.
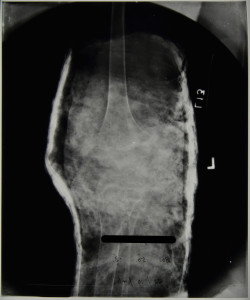
The collapse was maintained well into 1947 which involved her having refills of air every two weeks throughout this period. For the first three months she received refills of 200-300ccs of air at a time, progressing to 400ccs the month after, and then eventually 500-600ccs at a time. Figures 3-6 show the progression of the artificial pneumothorax as more air is inserted and the lung collapses further. Over time we can see that the cavity in the right mid zone collapses and closes, one of the main aims of the treatment. In early June 1946 a procedure was performed to divide adhesions between the lung and the chest wall which allowed the collapse to progress further. She was discharged in June 1947 with her condition described as improved.

17 Jan 1946
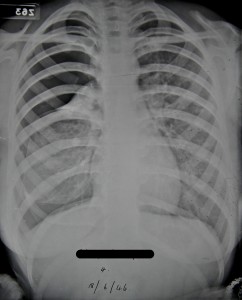
18 June 1946

2 Sept 1946

15 April 1947