Abdominal tuberculosis was a common diagnosis amongst the patients of Stannington Sanatorium and the patient case notes and radiographs give some indication as to the progression and manifestation of this form of TB. As was seen in the post from 19 November detailing the different types of TB, abdominal tuberculosis was a common extra-pulmonary form of the disease in which patients had often contracted the bovine strain of tuberculosis (mycobacterium-bovis) through the ingestion of unpasteurised or contaminated milk. We will explore the problems that arose from contaminated milk in a later post.
Abdominal TB most commonly affects the intestinal tract, mesenteric lymph nodes, and peritoneum and presents with symptoms such as abdominal pain, diarrhoea, rectal bleeding, and weight loss. The diagnosis of suspected extra-pulmonary forms of TB can often be assisted by chest x-rays where either active or healed tuberculous lesions can be seen. However in the case of abdominal TB where the primary point of infection is often not through the lungs but through the digestive system there may not be any evidence of any associated pulmonary infection. (Lambrianides et al, p.888) We don’t see as many radiographs within the Stannington records relating to abdominal tuberculosis in comparison to other manifestations of the disease such as pulmonary or bones and joints but there are nevertheless some good examples throughout the collection.
Case Study 1


The above radiographs are some of the earliest examples of abdominal TB from amongst the Stannington collection. They both relate to patient 80/21, a 9-year old female admitted in 1939 who presented with “vague abdominal signs and pain and traces of albumin in urine,” and a report on an x-ray taken prior to admission states that “calcified glands visible in abdomen above sacrum.” The reports given on the above two x-rays in the patient’s medical notes are very brief, with the first, figure one, being taken on 20 April 1939 and the report simply stating “gland to right of spine.” The second, figure two, was taken on 12 October 1939 and the report stated “calcification better seen in abdominal glands.”
Case Study 2

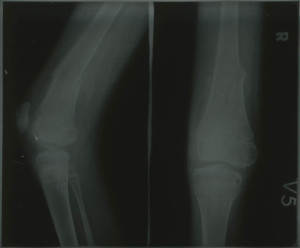
Figure 3 relates to a patient who was originally admitted in June 1940 as patient 86/46 and discharged in May 1941 only to be re-admitted some years later in September 1947 as patient 118/1947. On his first admission he was 5 years old and it was reported that during the past year he had had several attacks of vomiting and abdominal pain but an initial examination found no resistance in the abdomen and no mass was felt. No glands were seen in the x-rays of his abdomen taken at this time. The above radiograph was taken in October of 1947 following his second admission and the radiographic images from this slightly later period tend to be much clearer and better defined than those from the early 1940s, such as in figures 1 & 2. When he was admitted the second time he presented with “listlessness, poor appetite, vague abdominal pain & night sweats” but during his stay no evidence of any active disease was actually found, with the above x-ray showing calcified abdominal glands, presumably as a result of his previous, now quiescent, case of abdominal TB from 7 years earlier. He was discharged less than three months later once his symptoms had settled down.
There is little evidence of surgical treatments being employed in Stannington to treat abdominal tuberculosis, particularly in the earlier files. This is corroborated by early literature on abdominal TB in children where rest and sunshine are cited as the main methods of treatment alongside the prevention of the putrefaction of bowel contents by reducing the intake of meat and eggs and the administration of charcoal and the occasional dose of mercurial aperient. (Sundell, 1926) Later studies however recommend the use of surgical treatments to deal with intestinal lesions in order to prevent healing by fibrosis which could lead to obstructions causing later problems. (Kapoor & Sharma, 1988) This healing process is evident in the radiographs of patient 118/1947 showing the calcified glands, with the possibility of problems occurring later on in life being something to consider with many of the Stannington patients.
Sources
KAPOOR, V.K. & SHARMA, L.K. (1988) Abdominal Tuberculosis, British Journal of Surgery, 75 (1), pp.2-3
LAMBRIANIDES, A.L., ACKROYD, N. & SHOREY, B.A. (1980) Abdominal Tuberculosis, British Journal of Surgery, 67 (12), pp.887-889
SUNDELL, C.E. (1926) Abdominal Tuberculosis in Children, Postgraduate Medical Journal, 2 (14), pp.24-26